AI in Healthcare: Real Use Cases and Limitations
This comprehensive guide explores how artificial intelligence is transforming healthcare, from faster disease diagnosis to personalized treatment plans. We examine real-world AI applications already helping doctors and patients, including diagnostic tools that detect cancers earlier, AI systems that predict patient deterioration, and algorithms that accelerate drug discovery. The article also addresses crucial limitations: AI's need for massive datasets, potential biases in medical algorithms, regulatory challenges, and the irreplaceable role of human judgment in healthcare. Learn how AI complements rather than replaces medical professionals, what patients should know about AI health tools, and practical considerations for the future of medicine.
AI in Healthcare: Real Use Cases and Limitations
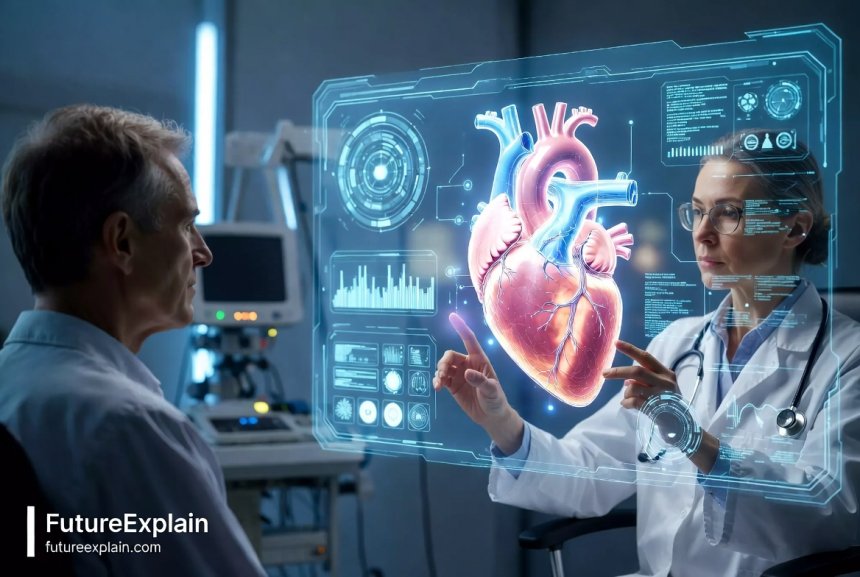
Artificial intelligence is transforming healthcare in ways that were science fiction just a decade ago. From algorithms that can detect diseases in medical scans to systems that predict patient outcomes, AI is becoming an essential tool in modern medicine. But what does this really mean for patients, doctors, and the healthcare system as a whole?
In this comprehensive guide, we'll explore the real applications of AI in healthcare today, separate hype from reality, and examine both the remarkable potential and important limitations of this technology. Whether you're a patient curious about AI-assisted diagnosis, a healthcare professional considering new tools, or simply interested in how technology is changing medicine, this article provides clear, balanced explanations.
How AI Is Different in Healthcare
Before diving into specific applications, it's important to understand what makes healthcare AI unique. Unlike AI in other fields like entertainment or finance, healthcare AI deals with human lives, requires exceptional accuracy, and operates under strict regulations. These systems must be not only intelligent but also reliable, explainable, and safe.
Healthcare AI typically falls into several categories: diagnostic AI that helps identify diseases, predictive AI that forecasts health outcomes, administrative AI that streamlines hospital operations, and therapeutic AI that assists in treatment planning. Each category has different requirements, validation processes, and regulatory pathways.
The development of medical AI follows rigorous scientific standards. Before any AI tool can be used in clinical settings, it undergoes extensive testing, validation against gold-standard methods, and regulatory review by bodies like the FDA in the United States or the EMA in Europe. This careful approach ensures patient safety but also means adoption happens more slowly than in other AI fields.
Real-World AI Applications in Healthcare Today
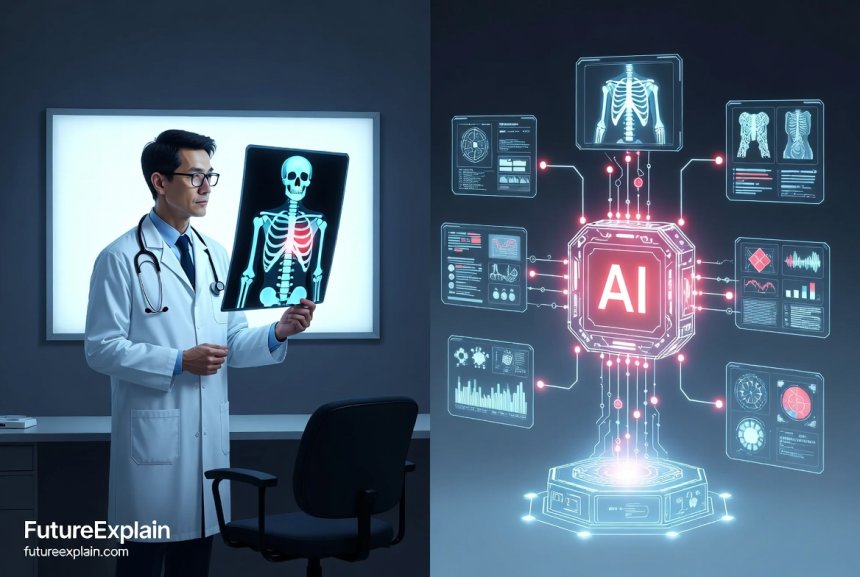
1. Diagnostic Assistance: Seeing What Humans Might Miss
One of the most developed areas of healthcare AI is diagnostic assistance. These systems help doctors detect diseases earlier and more accurately by analyzing medical images, lab results, and patient data.
Medical Imaging Analysis: AI algorithms can now analyze X-rays, CT scans, MRIs, and other medical images with remarkable accuracy. For example:
- Cancer detection: AI systems can identify suspicious lesions in mammograms, sometimes detecting breast cancer earlier than human radiologists. Studies show some algorithms reduce false negatives by up to 9.4% compared to human readers alone.
- Neurological conditions: AI helps detect early signs of Alzheimer's disease in brain scans years before symptoms become apparent.
- Eye disease screening: Algorithms can diagnose diabetic retinopathy and macular degeneration from retinal scans with accuracy matching ophthalmologists.
These systems don't replace radiologists but serve as "second readers" that highlight areas needing closer examination. As Dr. Katherine Lee, a radiologist at Johns Hopkins, explains: "The AI flags potentially concerning areas, but the final diagnosis and patient communication remain firmly in human hands."
2. Predictive Analytics: Preventing Problems Before They Occur
Predictive AI analyzes patient data to forecast health outcomes, allowing for early intervention. These systems examine electronic health records, vital signs, lab results, and even social determinants of health to identify patients at risk.
Hospital Readmission Prediction: Many hospitals now use AI to predict which patients are likely to be readmitted within 30 days of discharge. By identifying high-risk patients, care teams can provide additional support, follow-up, and monitoring to prevent unnecessary returns to the hospital.
Deterioration Prediction: In intensive care units and general hospital wards, AI systems monitor patient vital signs continuously, looking for subtle patterns that indicate impending deterioration. These "early warning systems" can alert nurses and doctors hours before a patient's condition becomes critical, allowing for timely intervention.
Chronic Disease Management: For conditions like diabetes, heart disease, and asthma, AI-powered apps and devices help patients manage their health. These tools analyze glucose readings, activity levels, medication adherence, and symptoms to provide personalized recommendations and alert healthcare providers when intervention is needed.
3. Drug Discovery and Development
The traditional drug discovery process takes 10-15 years and costs billions of dollars. AI is dramatically accelerating this timeline by:
- Identifying drug candidates: AI algorithms analyze biological data to identify molecules that might effectively target specific diseases
- Predicting drug interactions: Before expensive clinical trials, AI models predict how potential drugs will interact with the human body
- Optimizing clinical trials: AI helps design more efficient trials and identify suitable participants faster
During the COVID-19 pandemic, AI played a crucial role in accelerating vaccine development and identifying potential treatments. While AI doesn't replace laboratory work and clinical trials, it helps researchers prioritize the most promising candidates, saving time and resources.
4. Personalized Treatment Planning
Every patient is unique, and AI helps create truly personalized treatment plans by analyzing vast amounts of data about an individual's genetics, lifestyle, medical history, and treatment responses.
Oncology: In cancer treatment, AI systems analyze tumor genetics to recommend targeted therapies most likely to work for a specific patient's cancer type. This approach, sometimes called "precision oncology," has improved outcomes for certain cancers while reducing side effects from ineffective treatments.
Mental Health: AI-powered apps provide cognitive behavioral therapy techniques, mood tracking, and crisis support. While these don't replace human therapists, they offer accessible support between sessions and for those who can't access traditional therapy.
Surgical Planning: Before complex surgeries, AI creates 3D models from patient scans, allowing surgeons to plan procedures virtually. Some systems even suggest optimal surgical approaches based on similar successful cases.
Administrative and Operational AI in Healthcare
Beyond direct patient care, AI is transforming healthcare administration and operations:
Medical Documentation: AI-powered speech recognition and natural language processing help doctors create clinical notes more efficiently. These systems can extract relevant information from doctor-patient conversations and populate electronic health records automatically.
Insurance and Billing: AI streamlines insurance claim processing, reducing errors and speeding up reimbursements. It can also help identify billing irregularities and potential fraud.
Hospital Resource Management: AI algorithms predict patient admissions, helping hospitals optimize staffing, bed allocation, and equipment availability. This improves efficiency and reduces wait times.

The Limitations and Challenges of Healthcare AI
While AI offers tremendous potential, it's crucial to understand its limitations. Healthcare AI faces unique challenges that don't exist in other applications.
1. Data Quality and Quantity Requirements
AI systems require massive amounts of high-quality, accurately labeled data to train effectively. In healthcare, this presents several problems:
- Data silos: Patient data is often fragmented across different hospitals, clinics, and systems
- Privacy restrictions: Strict regulations like HIPAA limit data sharing for training AI models
- Data bias: If training data lacks diversity, AI systems may perform poorly for underrepresented populations
As noted in a 2023 study published in The Lancet Digital Health, many medical AI models are trained on data from wealthy, urban hospitals and may not generalize well to rural or low-resource settings.
2. The "Black Box" Problem
Many advanced AI systems, particularly deep learning models, are difficult to interpret. When an AI recommends a diagnosis or treatment, doctors need to understand why to make informed decisions. This "explainability" challenge is especially critical in healthcare where decisions affect human lives.
Researchers are developing more interpretable AI models and explanation techniques, but this remains an active area of investigation. As Dr. Marcus Chen, an AI ethics researcher at Stanford, explains: "A doctor can't simply tell a patient, 'The computer says you have cancer' without being able to explain the reasoning. Trust in medicine requires understanding."
3. Regulatory and Validation Challenges
Medical AI faces rigorous regulatory scrutiny, which is necessary for patient safety but slows deployment. The FDA has approved over 500 AI-enabled medical devices as of 2024, but each approval requires extensive validation.
The validation process presents unique challenges because:
- AI models may perform differently in real-world settings than in controlled studies
- Medical practice evolves, requiring AI systems to be updated and revalidated
- Different countries have varying regulatory requirements
4. Integration with Clinical Workflows
Successful healthcare AI must fit seamlessly into existing clinical workflows without adding burden to already-busy healthcare professionals. Poorly designed AI tools that interrupt workflows or generate excessive alerts can lead to "alert fatigue" and may be abandoned regardless of their technical capabilities.
The most effective AI tools are those designed in collaboration with clinicians from the beginning, addressing real clinical needs while respecting workflow constraints.
5. Liability and Responsibility Questions
When AI assists in medical decisions, questions arise about liability if something goes wrong. Is the doctor responsible for following or overriding an AI recommendation? What if the AI system itself has an error? These legal and ethical questions are still being resolved through legislation, court cases, and professional guidelines.
Most healthcare institutions using AI establish clear protocols about when and how clinicians should use AI recommendations, emphasizing that AI supports but doesn't replace professional judgment.
Ethical Considerations in Healthcare AI
The use of AI in healthcare raises important ethical questions that go beyond technical limitations:
Bias and Fairness: If AI systems are trained on biased data, they may perpetuate or even amplify healthcare disparities. For example, an algorithm trained primarily on data from white patients might be less accurate for patients of color. Addressing this requires diverse training data and ongoing monitoring for biased outcomes.
Privacy: Medical AI requires access to sensitive patient data. Robust privacy protections, transparent data practices, and patient consent are essential. Some promising approaches include federated learning, where AI models are trained across multiple institutions without sharing raw patient data.
Access and Equity: There's a risk that AI health tools could primarily benefit wealthy individuals and institutions, widening health disparities. Ensuring equitable access requires conscious effort in development, pricing, and deployment strategies.
Human Connection: Medicine involves empathy, compassion, and human connection—qualities AI cannot replicate. The most ethical applications of healthcare AI augment rather than replace human care, freeing clinicians to focus on aspects of medicine that require human touch.
What Patients Should Know About AI Health Tools
As AI becomes more common in healthcare, patients should be informed consumers. Here's what to know:
AI is an assistant, not a replacement: Even the most advanced AI tools support rather than replace healthcare professionals. Your doctor remains responsible for your care.
Ask questions: If AI is involved in your care, you have the right to ask how it's being used, what data it analyzes, and how it supports decision-making.
Be cautious with consumer health AI: While many health apps use AI, they vary widely in quality and validation. Look for apps developed with medical professionals and backed by clinical evidence.
Understand privacy policies: Before using any digital health tool, review its privacy policy to understand how your data will be used and protected.
The Future of AI in Healthcare
Looking ahead, several trends are shaping the future of healthcare AI:
Multimodal AI: Future systems will combine data from multiple sources—images, genetics, electronic records, wearable sensors—to provide more comprehensive insights. Learn more about this approach in our article on multimodal AI.
Edge AI in Medical Devices: AI will run directly on medical devices rather than in the cloud, enabling faster analysis and better privacy. This aligns with trends in TinyML and edge AI.
Continuous Learning Systems: Rather than static models, future healthcare AI will continuously learn from new data while maintaining safety through careful monitoring and validation.
Global Health Applications: AI has particular potential to improve healthcare in low-resource settings by providing diagnostic support where specialists are scarce. However, this requires models trained on relevant data and adapted to local conditions.
Practical Guidance for Healthcare Professionals
For doctors, nurses, and healthcare administrators considering AI tools:
Start with a problem, not a technology: Identify clinical or operational challenges before seeking AI solutions. The best AI tools solve specific, well-defined problems.
Evaluate evidence rigorously: Look for peer-reviewed studies demonstrating effectiveness in real-world settings similar to yours. Be skeptical of claims without solid validation.
Consider workflow integration: The most technically advanced tool may fail if it doesn't fit into clinical workflows. Involve end-users in evaluation and implementation.
Plan for ongoing monitoring: AI systems require continuous monitoring to ensure they perform as expected and adapt to changing conditions.
Maintain human oversight: Establish clear protocols for when and how clinicians should use AI recommendations, emphasizing that ultimate responsibility remains with healthcare professionals.
Conclusion: A Balanced Perspective on Healthcare AI
Artificial intelligence is transforming healthcare in profound ways, offering the potential for earlier diagnoses, more personalized treatments, and more efficient healthcare delivery. Real applications today are already improving patient outcomes and supporting overburdened healthcare systems.
However, healthcare AI also faces significant limitations and challenges. These systems require massive, diverse datasets; must integrate into complex clinical workflows; and raise important ethical questions about bias, privacy, and access. Most importantly, AI cannot and should not replace the human elements of medicine—compassion, judgment, and the doctor-patient relationship.
The most promising path forward is one of thoughtful integration, where AI augments human expertise rather than attempting to replace it. As healthcare continues to evolve, maintaining this balanced perspective—embracing innovation while respecting medicine's human foundations—will be essential for realizing AI's full potential to improve health for all.
For those interested in related topics, explore our articles on AI ethics and safety, future AI trends, and how AI helps different professions.
Share
What's Your Reaction?
 Like
1850
Like
1850
 Dislike
12
Dislike
12
 Love
420
Love
420
 Funny
35
Funny
35
 Angry
8
Angry
8
 Sad
15
Sad
15
 Wow
310
Wow
310

















What about the environmental impact of all this computing power for healthcare AI? Training large models requires significant energy - how does that balance against health benefits?
I'm a healthcare administrator, and we're implementing AI for scheduling and resource management. The predictive analytics for patient admissions has already reduced wait times by 15% in our emergency department.
The cost optimization potential is huge. If AI can reduce unnecessary tests and procedures, it could make healthcare more affordable. But will those savings be passed to patients or just increase profits?
How do medical professionals stay current with all these AI tools? The technology evolves faster than traditional medical education can keep up with.
As a patient with a rare genetic condition, I wish there was more AI research focused on rare diseases. Most AI seems trained on common conditions because there's more data available.
You've identified a real challenge, Levi. Rare diseases suffer from the "small data" problem. However, some researchers are using techniques like transfer learning (where models trained on common diseases are adapted for rare conditions) and federated learning (combining data from multiple institutions without sharing it) to address this. Patient advocacy groups are also helping collect data.
The article mentions wearable devices - I'm curious how accurate these consumer health devices really are compared to medical-grade equipment. Should people make health decisions based on their smartwatch data?