AI for Healthcare: Practical Use Cases and Limits
This comprehensive guide explores the transformative potential of artificial intelligence in healthcare while providing a balanced view of its limitations. We cover practical applications including diagnostic assistance, medical imaging analysis, drug discovery acceleration, and personalized treatment planning. The article provides a beginner-friendly roadmap for implementation, discusses regulatory considerations, and addresses ethical challenges. Unlike overly optimistic or critical perspectives, we offer a balanced view showing both what AI can achieve today and where human expertise remains irreplaceable. Includes real-world case studies, implementation checklists, and guidance for healthcare professionals seeking to integrate AI responsibly.

Introduction: The AI Revolution in Healthcare
Artificial intelligence is transforming healthcare in ways that seemed like science fiction just a decade ago. From AI-powered diagnostic tools that can detect diseases earlier than human experts to algorithms that predict patient outcomes with remarkable accuracy, the potential seems boundless. Yet, alongside these exciting developments come important questions about limitations, ethics, and practical implementation. In this comprehensive guide, we'll explore both the practical applications of AI in healthcare and the very real boundaries of what current technology can achieve.
Healthcare represents one of AI's most promising and challenging application domains. Unlike other industries where errors might mean lost revenue or inconvenience, healthcare mistakes can literally be matters of life and death. This creates unique requirements for accuracy, transparency, and accountability. As we'll see throughout this article, the most successful AI healthcare implementations recognize this reality, positioning AI as an assistive tool rather than a replacement for human expertise.
This article is designed for healthcare professionals, administrators, technologists, and curious patients who want to understand what AI can realistically achieve in medical settings today. We'll move beyond the hype to examine concrete use cases, implementation challenges, and the critical limitations that every healthcare organization must understand before adopting AI solutions.
Understanding Healthcare AI: Core Concepts for Beginners
Before diving into specific applications, let's establish some fundamental concepts. Healthcare AI isn't a single technology but rather a collection of approaches including machine learning, natural language processing, computer vision, and predictive analytics. Each of these has distinct applications in medical settings.
Machine Learning in Healthcare: At its simplest, machine learning involves algorithms that improve automatically through experience. In healthcare, this might mean systems that get better at identifying tumors in medical images as they process more scans, or algorithms that refine their predictions about patient readmission risk based on historical data.
Natural Language Processing (NLP): NLP enables computers to understand, interpret, and generate human language. In healthcare, this powers everything from chatbots that triage patient symptoms to systems that extract structured information from unstructured clinical notes.
Computer Vision: This AI capability allows machines to interpret and understand visual information. In medical settings, computer vision algorithms analyze everything from X-rays and MRI scans to microscopic tissue samples and surgical video feeds.
Predictive Analytics: These systems use historical data to predict future outcomes. Healthcare applications include predicting which patients are at highest risk for complications, forecasting disease outbreaks, or estimating hospital bed occupancy.
Practical Use Case 1: Diagnostic Assistance and Medical Imaging
One of AI's most proven healthcare applications is in diagnostic assistance, particularly in medical imaging. Research shows that AI algorithms can now match or even exceed human radiologists in detecting certain conditions from medical images. However, the key word here is "assistance" – these systems work best when combined with human expertise.
How AI Medical Imaging Works
AI systems for medical imaging typically work through a process called supervised learning. They're trained on thousands or even millions of labeled medical images – for example, X-rays marked by radiologists as either showing pneumonia or not. The algorithm learns to recognize patterns associated with the condition, gradually improving its accuracy.
Once trained, these systems can analyze new images in seconds, highlighting areas of concern for human review. This doesn't replace radiologists but rather augments their capabilities, allowing them to focus attention where it's most needed and potentially catching subtle signs that might otherwise be missed.
Real-world examples include Google's DeepMind system for detecting eye diseases from retinal scans, which has shown remarkable accuracy in clinical trials. Similarly, numerous companies now offer AI-powered tools for detecting breast cancer in mammograms, with studies showing these systems can reduce false negatives by up to 9.4%.
Implementation Considerations
Implementing AI imaging systems requires careful planning. Organizations must consider:
- Integration with existing systems: Most healthcare facilities use Picture Archiving and Communication Systems (PACS) for storing and viewing medical images. AI tools need to integrate seamlessly with these systems.
- Validation and regulatory approval: In most countries, AI diagnostic tools require regulatory approval (like FDA clearance in the United States).
- Workflow integration: How will AI findings be presented to clinicians? Will they appear as overlays on images, separate reports, or integrated into electronic health records?
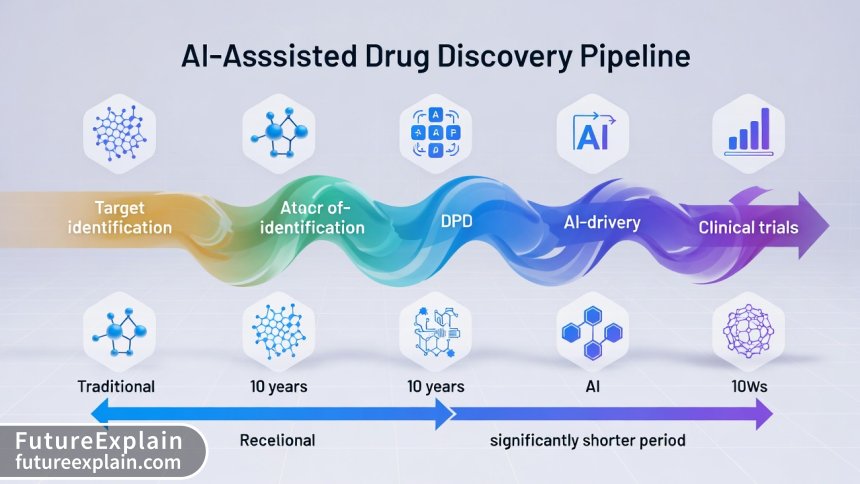
Practical Use Case 2: Drug Discovery and Development
The traditional drug discovery process is notoriously slow and expensive, typically taking 10-15 years and costing billions of dollars from initial discovery to market approval. AI is dramatically accelerating this process by helping identify promising drug candidates faster and with higher precision.
AI in Early-Stage Discovery
AI algorithms can analyze vast databases of chemical compounds, biological targets, and clinical trial data to identify potential drug candidates that human researchers might overlook. These systems use techniques like:
- Virtual screening: Testing millions of compounds against target proteins using computational models
- De novo drug design: Generating entirely new molecular structures optimized for specific therapeutic targets
- Predicting drug-target interactions: Forecasting how potential drugs will interact with biological systems
Companies like Exscientia and BenevolentAI have used these approaches to reduce early-stage drug discovery from years to months. For example, Exscientia developed a potential treatment for obsessive-compulsive disorder in less than 12 months – a process that traditionally takes 4-5 years.
Clinical Trial Optimization
AI also optimizes later stages of drug development. Algorithms can:
- Identify ideal patient populations for clinical trials
- Predict which patients are most likely to respond to treatments
- Monitor trial participants in real-time for adverse effects
- Analyze trial data more efficiently to identify signals of efficacy or safety concerns
Practical Use Case 3: Personalized Treatment Planning
One of healthcare's oldest challenges is that the same treatment can produce dramatically different results in different patients. AI is helping move medicine from one-size-fits-all approaches to truly personalized care based on individual genetics, lifestyle, and medical history.
Precision Oncology Leading the Way
Cancer treatment has been at the forefront of personalized medicine, and AI is taking this to new levels. Systems like IBM Watson for Oncology (despite its well-publicized challenges) demonstrated the concept of analyzing a patient's genetic profile alongside thousands of research papers and clinical guidelines to suggest treatment options.
More successful implementations include tools that:
- Analyze tumor genetics to predict which treatments will be most effective
- Monitor treatment response in real-time through imaging and biomarker analysis
- Adjust treatment plans based on how individual patients are responding
Chronic Disease Management
For chronic conditions like diabetes, heart disease, and respiratory illnesses, AI-powered systems can create highly personalized management plans. These might include:
- Customized medication regimens based on individual metabolism and genetics
- Personalized diet and exercise recommendations
- Real-time monitoring and adjustment based on continuous glucose monitors, wearable devices, or patient-reported outcomes
Practical Use Case 4: Administrative Automation and Operational Efficiency
While diagnostic and treatment applications get most attention, some of AI's most immediate benefits in healthcare come from administrative and operational applications. These areas often face fewer regulatory hurdles and can deliver quick returns on investment.
Medical Documentation and Coding
Healthcare providers spend enormous time on documentation and medical coding. AI-powered natural language processing can:
- Transcribe clinical encounters automatically
- Extract structured data from unstructured clinical notes
- Suggest appropriate medical codes for billing and compliance
- Identify documentation gaps or inconsistencies
Tools like Nuance's Dragon Ambient eXperience (DAX) demonstrate this application, using AI to listen to patient encounters and automatically generate clinical notes, reducing documentation burden by up to 50% according to company data.
Hospital Operations Optimization
AI algorithms can optimize numerous hospital operations including:
- Patient flow prediction: Forecasting emergency department volumes, inpatient admissions, and discharges
- Resource allocation: Optimizing staff scheduling, operating room utilization, and equipment deployment
- Supply chain management: Predicting medication and supply needs, reducing waste while preventing shortages
Practical Use Case 5: Telemedicine and Remote Patient Monitoring
The COVID-19 pandemic accelerated telemedicine adoption, and AI is enhancing these virtual care models. AI-powered telemedicine goes beyond simple video consultations to include sophisticated remote monitoring and triage capabilities.
AI-Enhanced Telemedicine Platforms
Modern telemedicine platforms incorporate AI to:
- Triage patients based on symptom severity and urgency
- Guide patients through self-examination using smartphone cameras
- Analyze voice patterns for potential neurological or respiratory conditions
- Provide real-time language translation for multilingual consultations
Companies like Babylon Health and Teladoc have integrated various AI capabilities into their platforms, though with mixed results that highlight both potential and limitations.
Remote Patient Monitoring Systems
AI transforms remote monitoring from simple data collection to intelligent analysis. Systems can:
- Continuously analyze data from wearable devices (heart rate, activity, sleep patterns)
- Detect subtle changes that might indicate health deterioration
- Alert healthcare providers only when intervention is truly needed (reducing alert fatigue)
- Provide personalized feedback and coaching to patients between visits
The Critical Limits of Healthcare AI
While the applications above demonstrate AI's potential, understanding its limitations is equally important. These boundaries define what AI can and cannot do in healthcare today and for the foreseeable future.
Limitation 1: Data Quality and Availability
AI systems are only as good as the data they're trained on. Healthcare data presents unique challenges:
- Data fragmentation: Patient information is scattered across multiple systems that don't communicate well
- Data quality issues: Medical records often contain errors, inconsistencies, and missing information
- Bias in training data: If AI is trained primarily on data from certain demographic groups, it may perform poorly for others
- Privacy restrictions: Healthcare data is highly protected, making it difficult to assemble the large, diverse datasets AI needs
These data challenges mean that AI systems developed in research settings often struggle when deployed in real clinical environments with messier, more complex data.
Limitation 2: The "Black Box" Problem
Many advanced AI systems, particularly deep learning models, are essentially "black boxes" – they can make accurate predictions but can't explain how they reached their conclusions. In healthcare, where decisions have serious consequences, this lack of explainability is a major barrier.
Consider a scenario where an AI system recommends against a particular treatment for a cancer patient. If doctors can't understand why – Is it because of drug interactions? Genetic factors? Comorbidities? – they're unlikely to trust or follow the recommendation, regardless of its potential accuracy.
Research in explainable AI (XAI) is addressing this challenge, but truly transparent healthcare AI remains largely aspirational rather than realized.
Limitation 3: Regulatory and Liability Challenges
Healthcare is one of the most heavily regulated industries, and AI introduces new regulatory complexities:
- Classification challenges: Is an AI diagnostic tool a medical device? Software? Both? Regulatory frameworks are still catching up.
- Validation requirements: How do you validate an AI system that continues learning and changing after deployment?
- Liability questions: If an AI system makes an error that harms a patient, who is responsible? The developer? The healthcare provider who used it? The institution that purchased it?
These regulatory uncertainties slow AI adoption as healthcare organizations wait for clearer guidelines and precedents.
Limitation 4: Integration with Clinical Workflows
Healthcare providers are already overburdened with administrative tasks and complex technology systems. Adding AI tools that don't integrate seamlessly into existing workflows creates more problems than it solves.
Successful AI implementation requires:
- Minimal additional clicks or steps for clinicians
- Clear presentation of AI insights without information overload
- Alignment with existing clinical processes and decision-making patterns
- Adequate training and support for healthcare staff
Many AI healthcare projects fail not because the technology doesn't work, but because it disrupts rather than enhances clinical workflows.
Limitation 5: The Human Element of Healthcare
Perhaps AI's most fundamental limitation in healthcare is its inability to replicate the human elements of care – empathy, intuition, contextual understanding, and the therapeutic value of human connection.
Consider these scenarios where human judgment remains irreplaceable:
- Understanding a patient's social context and how it affects treatment adherence
- Recognizing when a patient isn't telling the whole story due to embarrassment or fear
- Making ethical decisions when treatment options involve quality-of-life tradeoffs
- Providing comfort and emotional support during difficult diagnoses or treatments
These human elements aren't just "nice to have" – they're essential components of effective healthcare that AI cannot replicate.
Implementation Roadmap: Getting Started with Healthcare AI
For healthcare organizations considering AI adoption, a thoughtful, phased approach is essential. Here's a practical roadmap based on successful implementations.
Phase 1: Assessment and Planning
Before purchasing any AI solution, conduct a thorough assessment:
- Identify priority areas: Where could AI provide the most value? Focus on areas with clear pain points and measurable outcomes.
- Assess data readiness: Do you have the necessary data in usable formats? Is it sufficiently clean and comprehensive?
- Evaluate organizational readiness: Do staff have the necessary technical skills? Is leadership committed to the initiative?
- Understand regulatory requirements: What approvals will be needed for your planned applications?
Phase 2: Pilot Projects
Start with small, focused pilot projects rather than enterprise-wide deployments:
- Choose applications with clear success metrics
- Select areas with lower risk and regulatory burden initially
- Involve end-users (clinicians, administrators) from the beginning
- Plan for rigorous evaluation of both technical performance and workflow impact
Phase 3: Scaling and Integration
Based on pilot results, develop a scaling plan:
- Address issues identified during pilots
- Develop training programs for broader rollout
- Establish ongoing monitoring and maintenance processes
- Create governance structures for AI decision-making and oversight
Ethical Considerations in Healthcare AI
Beyond technical limitations, healthcare AI raises profound ethical questions that organizations must address.
Algorithmic Bias and Health Equity
AI systems can perpetuate and even amplify existing healthcare disparities if not carefully designed. Examples include:
- Skin disease detection algorithms trained primarily on lighter skin tones performing poorly on darker skin
- Predictive models for healthcare needs trained on data from well-served populations failing in underserved areas
- Language models that don't understand medical terminology in different languages or dialects
Mitigating bias requires diverse training data, rigorous testing across population subgroups, and ongoing monitoring for disparate impacts.
Privacy in the Age of AI
AI systems often require access to sensitive health data, creating privacy challenges:
- How is patient data protected during AI training and operation?
- Can AI insights be generated without exposing raw patient data?
- How do patients provide meaningful consent for AI uses of their data?
Techniques like federated learning (training AI across decentralized devices without sharing raw data) and differential privacy (adding mathematical noise to protect individual data points) offer potential solutions, but practical implementation remains challenging.
Autonomy and Human Oversight
As AI systems become more capable, questions arise about appropriate levels of human oversight. Should AI ever make autonomous healthcare decisions? Most experts agree that for the foreseeable future, AI should augment rather than replace human judgment in critical healthcare decisions.
Establishing clear guidelines for human oversight – when AI recommendations require confirmation, when they can be followed automatically, and who bears ultimate responsibility – is essential for ethical implementation.
Future Trends and Developments
Looking ahead, several trends will shape healthcare AI's evolution:
Multimodal AI Integration
Future systems will combine multiple data types – imaging, genomics, clinical notes, wearable data – for more comprehensive analysis. Rather than separate AI tools for different data types, integrated systems will provide holistic patient insights.
Edge AI for Real-Time Processing
Processing AI directly on medical devices (edge computing) will enable real-time analysis without cloud dependency. This is particularly important for time-sensitive applications like surgical assistance or critical care monitoring.
Generative AI in Healthcare
While still early, generative AI models show promise for tasks like synthesizing patient education materials, generating clinical trial protocols, or creating synthetic medical data for research while protecting patient privacy.
Regulatory Evolution
Regulatory frameworks will continue evolving to better accommodate AI's unique characteristics, potentially including approaches for continuous validation of learning systems and clearer liability guidelines.
Conclusion: Balancing Optimism with Realism
AI holds tremendous promise for transforming healthcare – improving diagnostic accuracy, personalizing treatments, accelerating drug discovery, and enhancing operational efficiency. The use cases we've explored demonstrate real, measurable benefits already being realized in clinical settings worldwide.
Yet, as we've also seen, AI has significant limitations. Data challenges, regulatory complexities, integration difficulties, and fundamental boundaries in replicating human judgment mean that AI will augment rather than replace healthcare professionals for the foreseeable future.
The most successful healthcare organizations will approach AI with balanced optimism – embracing its potential while respecting its limits. They'll start with focused applications that address clear pain points, involve clinical stakeholders throughout the process, and maintain appropriate human oversight of AI-assisted decisions.
As AI continues evolving, ongoing dialogue between technologists, clinicians, patients, regulators, and ethicists will be essential to ensure these powerful tools serve humanity's health needs responsibly and equitably. The future of healthcare isn't AI replacing humans, but humans and AI working together to achieve what neither could accomplish alone.
Further Reading
- AI in Healthcare: Real Use Cases and Limitations (Our 2024 foundation article)
- AI for Agriculture: Smart Farming & Crop Management (Cross-industry AI applications)
- Ethical AI Explained: Why Fairness and Bias Matter (Essential ethics background)
Visuals Produced by AI
Share
What's Your Reaction?
 Like
15234
Like
15234
 Dislike
187
Dislike
187
 Love
2345
Love
2345
 Funny
456
Funny
456
 Angry
123
Angry
123
 Sad
89
Sad
89
 Wow
2987
Wow
2987














As a bedside nurse for 25 years, I've seen many technology promises come and go. What I appreciate about this article is the recognition that technology should support, not replace, the human aspects of care. The most advanced AI can't replace a compassionate touch or experienced intuition.
This is one of the most balanced articles I've read on healthcare AI. Most are either hype or fearmongering. The practical implementation advice is especially valuable for those of us actually trying to deploy these technologies.
The future trends section got me thinking about multimodal AI. As an emergency physician, I'd love a system that could integrate vitals, imaging, lab results, and even voice stress analysis for a more complete patient picture. We're not there yet, but the direction is exciting.
I work in health insurance, and we're exploring AI for claims processing. The potential for reducing administrative costs is huge, but the article's warning about workflow disruption is spot on. We piloted one system that actually increased processing time because it didn't integrate with existing systems.
Chloe, we had similar experiences. What finally worked was building the AI around existing human processes rather than trying to replace them. The AI now pre-processes claims and flags exceptions for human review, rather than trying to fully automate everything.
The telemedicine AI section resonated. During the pandemic, we implemented an AI symptom checker that reduced unnecessary ER visits by 30%. But we learned the hard way about the importance of clear disclaimers - patients need to understand it's guidance, not diagnosis.
As a patient advocate, I worry about algorithmic determinism - when AI predictions become self-fulfilling prophecies. If an algorithm predicts poor outcomes for certain patients, might they receive less aggressive care, thus ensuring the poor outcome?
Anika, this is a profound concern that researchers are starting to address. Some are developing "counterfactual fairness" approaches where algorithms are trained to provide the same recommendations regardless of sensitive attributes. Ongoing auditing and human oversight remain essential.